FAQ: “When is strabismus surgery necessary? What should I be vigilant about before going through with it?” – A guide based upon what I would have wanted to know before undergoing eye muscle surgery
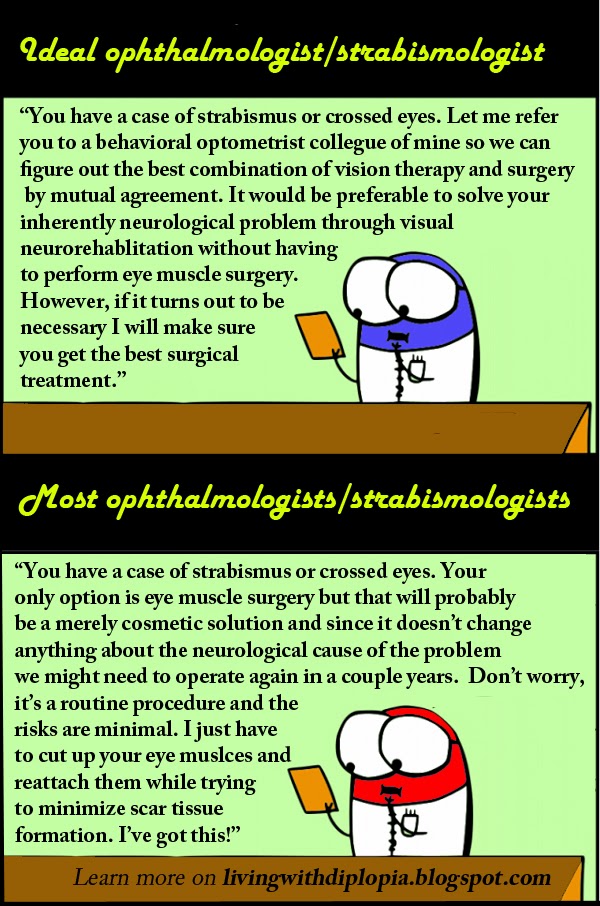
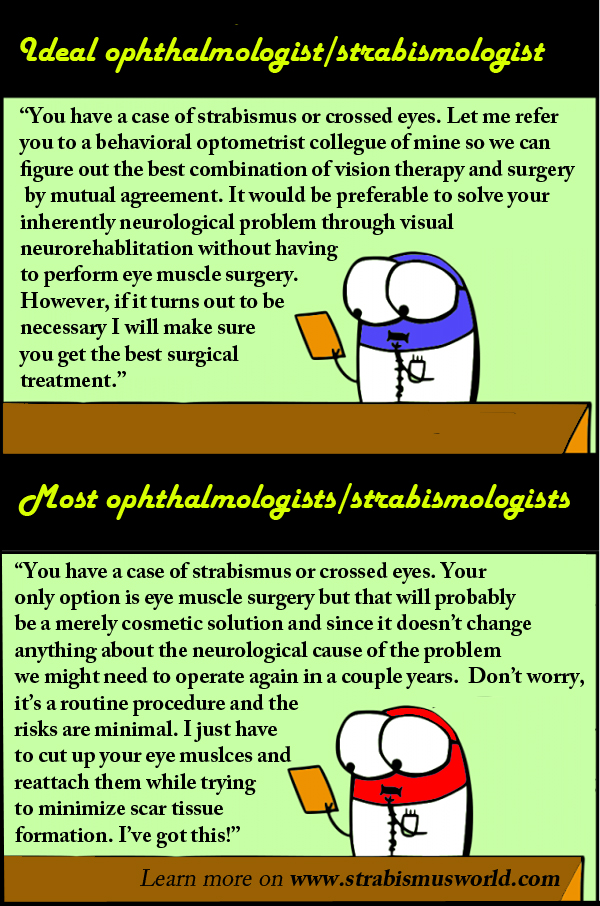
NOTICE: Because communication and collaboration between ophthalmologists/strabologists and developmental optometrists is generally poor, it’s hard to know whether one is getting the appropriate information or advice. Having suffered from strabismus for twenty years during which I have undergone three strabismus surgeries and more recently three years of Vision Therapy, I feel like my ideas might be useful to many who are struggling to make the right decision. I am not an optometrist or vision care professional but under the force of circumstances I have become well-read on the subject. Moreover, during this time, I have had lots of contact with other adult patients and parents of cross-eyed children. This blog entry is not clear cut advice, but it definitely contains elements to consider before undergoing eye muscle surgery and I hope it will lead to more informed decisions and a better life for everyone involved.
I’m not an anti-surgery zealot but it is safe to say that nowadays it is widely overused as a treatment for strabismus, often not in the patient’s interest. Even though often called a ‘routine procedure’ by surgeons, strabismus surgery is a serious life changing event. In order for the outcome to be beneficial, a cost-benefit analysis has to be made based on ALL available information. The effects of surgery are not easily undone so you want them to be positive. First of all you should be aware of all strabismus treatment options, which is often the first major stumbling block in dealing with the vision care sector. SURGERY IS NOT THE ONLY OPTION.
But once knowing the various options, who to believe? What to decide? I will try to be as objective as possible and give you my view on several strabismus situations one might encounter.
INTERMITTANT STRABISMUS/ PHORIAS
NEVER get surgery if your eyes are aligned some of the time but alignment can not be sustained during visually taxing tasks like reading. Nothing good will come of it. Take your healthy eyes and eye muscles and improve your vision and eye teaming skills through visual training until you are able to maintain eye alignment 100% of the time, also while reading. This can often be achieved in less than one year.
MANIFEST STRABISMUS/TROPIAS
INFANT: In case of strabismus, it is often said that ‘the sooner the surgery, the better’. This makes sense because in that case the baby will adapt more easily to the new artificially manufactured eye posture. But on the other hand, given the fact that an infant can adapt so easily it might be worth considering to avoid the surgery all together and opt for strengthening the visual system through stimulation. Infants are very malleable and have tremendous rebound capacity even when born cross-eyed. I would like to refer you to an earlier blog entry on this topic titled ‘I have a cross-eyed infant/child, what the hell am I supposed to do?’. Stimulation can include visual training and life style changes, Syntonics and physical therapy to aid with sensory motor development.
That being said I understand it sometimes feels ‘impossible’ to parents, especially when their child was born cross-eyed. It’s like it was always been this way and all around they get told it’s not possible to change the situation. As I see it, those children are born into a more difficult ‘visual position’ and it might be more challenging but they have the potential to develop normal vision like everyone else. The prevailing negativity among many vision care professionals often doesn’t help in moving towards that goal. Because other options are not offered or insufficiently tried (patching by itself is not a worthy equivalent to proper Vision Therapy), parents often feel like they have to act NOW and agree to surgery.
In theory, it sounds good. The child is still young and then at least cosmetically the issue is off the table. However, strabismus is NOT a cosmetic issue, it’s a functional issue. So if you agree to surgery, keep in mind you will have to stimulate the child’s brain and teach him to use both eyes together. Surgery should always come with recommended follow-up Vision Therapy. After rearranging the mechanics, you need to provide the little brain with ‘driving instructions’. Vision develops throughout childhood and its development has to be monitored carefully, especially in children starting out in a visually precarious situation. Vision development is an ongoing process which often does not easily lend itself to ‘quick fix solutions’.
Without these ‘driving instructions’ the eyes will often revert back to crossing leading to follow-up surgeries. Now, the thing that strabismus has going for it is usually the fact that in essence the eyes are healthy and the brain ‘just’ needs to learn how to control and use them. So the last thing you want to do is to actually damage the eyes or its surrounding muscles by cutting them up and reattaching them one or several times. So if you were to opt for surgery, and this piece of advice is based on my own personal experience, I strongly urge you to look for the best surgeon around. Do your due diligence. As in any profession, not all surgeons are created equal. Strabismus surgery is no small matter. Check it out on Youtube if you don’t believe me. You don’t go in there and come out the next day ‘That was fun! What’s next!? Otra cosa mariposa!’. A good surgeon will minimize damage and scar tissue while optimizing eye motility and posture which will allow the child to develop his vision further as optimally as possible. If dealing with an honest and knowledgeable surgeon he might admit that in many cases the best way to do that is not to perform surgery at all.
This brings me to another important point. Do not act on the opinion of one eye doctor or surgeon alone. Make sure to get the opinion of someone qualified in visual neurorehabilitation or vision therapy too. Sometimes these people are hard to find but it’s well worth it.
CHILDREN: For somewhat older children the same cost benefit analysis applies, with the difference that the child can to some extend choose or be compelled to cooperate in his own rehabilitation. Given the fact they are more or less consciously aware of what is happening I would rather try VT over surgery. Surgery often has a shock and awe effect by basically creating a dis-accord between the way the brain had developed so far and the new eye posture which is hard to predict. Surgery comes with certain risks and afterwards Vision Therapy will most likely still be necessary. Everyone reacts to surgery differently but you want to keep in mind visual rehabilitation is harder if the muscles have been cut up and reattached. Children still have very plastic brains and a surprisingly resilient body so you want to take advantage of that and thoroughly try Vision Therapy before resorting to surgery. In the long run, the functional benefits of good binocular vision are invaluable.
TEENAGERS are often more self-aware and motivated to straighten their eyes. If I would have been told of the option of VT when I was a teenager I would have grabbed it with both hands and would never have let go. Another important thing to mention is that vision development should get precedence over school work regardless of age. If there are just not enough hours in a day or it’s too stressful, you take care of the vision issue first. Vision is a prerequisite for good school performance so you want to start with that. First things first.
I had my surgeries at the ages of 16, 18 and 19. The third one was to make up for the second one and after that I was STILL not properly informed about all my options. These are delicate ages to get into the surgery adventure without knowing about visual rehabilitation and I was getting very, very desperate. I hope you read this before that happens. My esotropic brain underwent severe shock and awe after being forced to deal with an exotropic-ish eye posture with serious eye motility restrictions. I could not even maintain a stable gaze anymore and experienced constant double vision. My functionality suffered tremendously and I had to ‘relearn’ a lot of things. The consequences of those interventions are felt to this day. This is why I feel very strongly about informing patients of their options.
So ADULTS, when do you decide to go for surgery?
With the help of prism glasses surgery outcomes can be more or less simulated in advance (same goes for children and teenagers by the way).
1. If with the help of prisms you can achieve binocular sensory fusion in the brain, your problem is to a great extent of a mechanical nature. Two options come to mind.
– Get an appropriate pair of prism glasses which stabilize your gaze and allows for sensory fusion on a cortical level. The prism glasses function like crutches to artificially compensate for poor eye alignment. While using this kind of help, it is advisable to engage in visual rehabilitation and gradually decrease your need for these ‘crutches’. It will take a while but if the prism glasses are fairly comfortable this allows for a gradual transition without ‘shock and awe’.
– Try to fix the mechanical eye muscle problem by means of surgical intervention. If you achieved good sensory fusion with the prisms, a mechanical change through surgery might just fix the problem. In theory this sounds good and it can work. Much depends on the surgeon and on how well the surgery went. Have you not only have achieved eye alignment but is eye muscle damage minimized and eye motility optimized? You don’t want an ‘aligned’ eye just pointing forward unable to move appropriately and function in accordance with the other eye. Depending on the patient, this might lead to very annoying double vision. That being said, I personally know someone who experienced fusion through prisms, underwent eye muscle surgery by a very good strabologist and came out with full blown stereo vision. I have heard similar stories over the years with the appropriate amount of jealousy. 😉 This is to say the ‘shock and awe’ effect is not always negative but you need a really good surgeon and in my opinion it’s much more of a gamble than the prism + VT approach. Vision training might still be advisable after surgery. I have not gone into the financial costs of either option but if you do your research you will find that surgery is not only riskier but also more expensive.
2. Adults with stong suppression of one eye who don’t achieve immediate sensory fusion with prisms.
In this case the problem is not ‘merely mechanical’ and eye muscle surgery without Vision Therapy afterwards won’t really improve your vision. So let’s look at the options.
– You could, depending on your priorities, want to get cosmetic alignment at all costs without regard for functional vision and undergo surgery thinking that then at least you have already fixed the mechanical and cosmetic side of things. Problems with this approach might be that this is unlikely to stick if not structurally accommodated by the brain through vision therapy. Again, the risk of irreversible eye muscle damage should be considered along with other risks such as post-op double vision. You always want to remember that the problem is not really situated at the eye level but at the brain level so surgery will not solve the brain problem and might actually damage the eye muscles which weren’t really the problem in the first place.
– You could go down a less intrusive road of Vision Therapy focusing on gradually teaching your brain to point your eyes correctly and then gradually break through suppression in order to achieve sensory fusion and stereo vision. This is probably the less expensive and less risky road of the two, EVEN if not covered by health insurance. Outcomes will likely be better and more durable.
3. Adults whose suppression has been broken, experience double vision daily and don’t achieve sensory fusion but rather superimposed images through prisms.
This is a red flag and a behavioral/developmental optometrist should be consulted asap. Double vision has serious implications for quality of life and should be treated by neuro-rehabilitative methods without additional damage to the eyes or eye muscles. If no comfortable situation can be achieved with prisms, surgery will not be beneficial. In this case surgery is only a ‘good idea’ to make up for previous surgery debacles which should not have happened to begin with. So step away from the surgeon!
In this case the seriousness of the situation should be understood and every action should be aimed at improving rather than deteriorating this brain injury. Visual rehabilitation should take priority because otherwise the downward spiral will not be sustainable over the long haul. Vision Therapy programs should be aimed at resolving double vision through eye alignment, eventually leading to sensory fusion. Vision therapy will be less difficult, but not easy, without recent surgical trauma.
CONCLUSION
It would be unreasonable to completely discard the uses of eye muscle surgery since every case is different and requires a different treatment strategy. Nonetheless, surgery should be a measure of last resort. Many other more structural, less risky approaches should be tried first: Vision Therapy, Syntonics, … A good indication of how binocular vision problems (strabismus) and amblyopia (lazy eye) are brain problems, and generally not eye muscle problems, are recent studies using tDCS (transcranial Direct Current Stimulation) to promote fusion in the visual cortex in conjunction to vision therapy. It seems like a very promising method aimed at dealing with the real cortical problem rather than the cosmetic surface. It is also less invasive and risky than surgery, however crazy that may sound. More on this later.
So to sum up, I’m not saying ‘don’t get surgery under any circumstances’. I am just asking you to carefully weigh pros and cons and to not blindly follow one doctor or be pressured into surgery. Strabismus treatment or the pursuit of good functional binocular vision is more than just a medical issue. It’s also an educational, academic and work performance related issue. This makes it a socio-economic and ultimately democratic issue. Do we really want to provide good functional vision care and thus provide people with equal opportunities? Or do we just want to pretend to care and provide half measures leading nowhere but more medical bills and repeat cosmetic surgeries?
LAST WORD
“If you make something a little bit better, people might pay you for it; they may not. But if you make the world (or people’s lives) a radically better place, the money is going to come find you, in a fair and elegant way.” – Astro Teller
The content of this blog is based on twenty years of unpleasant experience and much hard work to undo past mistakes. If this and other blog entries helped you to avoid making similar mistakes and you can afford it, show some love by donating a few bucks. Thank you!
This comment has been removed by a blog administrator.
Thanx for sharing such a helpful article. This is written very well you are a very good writer. I am agree with you. Hope you will Carry own writing in the same way. Thumbs Up!
Taking Care of Your Vision